Concussions and repeated head injuries are no longer considered just occupational hazards linked to contact sports; they are now recognized as serious health problems.
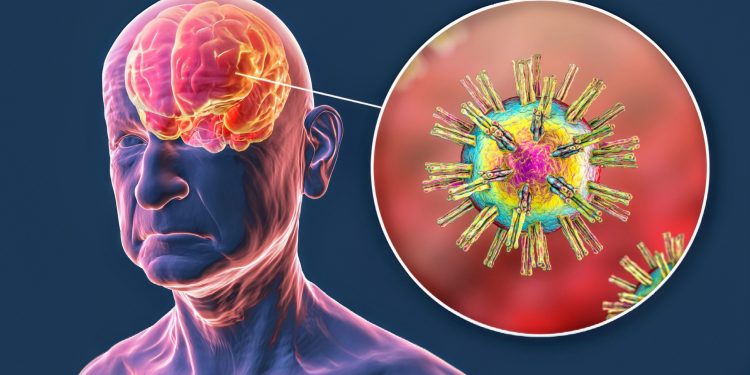
Recent research from Tufts University and the University of Oxford reveals a potential link between head trauma and the activation of dormant viruses in the brain, which could lead to long-term neurodegenerative diseases such as of Alzheimer’s.
The results, published in the journal Scientific signagesuggest that early preventive treatments using antiviral drugs could help mitigate these risks.
Hidden threat of dormant viruses
Our bodies harbor many dormant viruses, including herpes simplex virus 1 (HSV-1) and varicella zoster virus, which typically reside in neurons and glial cells without causing damage.
Dana Cairns, lead author and research associate in the Department of Biomedical Engineering at Tufts University, explained her previous findings.
“In this study, another virus – chickenpox – created the inflammatory conditions that activated HSV-1. We thought: What would happen if we subjected the brain tissue model to a physical disturbance, something akin to a concussion? Would HSV-1 wake up and trigger the process of neurodegeneration?
This question motivated the new study, which investigates how concussions might trigger these latent viruses.
Mimic brain trauma in the laboratory
To explore this, researchers developed a unique model of brain tissue. This model is a 6mm wide donut-shaped sponge made of silk proteins and collagen, infused with neural stem cells.
The stem cells transformed into neurons and glial cells, forming a network similar to that of a real brain, and some even harbored dormant HSV-1. The team simulated a concussion by enclosing the model in a cylinder and delivering a sudden jolt with a piston.
After subjecting the tissues to this controlled shock, Cairns observed that in models containing HSV-1, the virus reactivated.
Following this reactivation, the tissue began to exhibit key markers of Alzheimer’s disease: amyloid plaques, tau protein tangles, inflammation, neuronal death and increased numbers of glial cells – a condition known as gliosis. Repeated shocks intensified these effects.
In contrast, tissue models without HSV-1 showed only minor gliosis and no other indicators of Alzheimer’s.
Concussions and dormant viruses
The results clearly indicate that concussions could awaken dormant viruses in the brain, potentially leading to neurodegenerative conditions over time.
“This opens the question of whether antiviral drugs or anti-inflammatory agents might be useful as early preventive treatments after head injury to stop HSV-1 activation and reduce the risk of Alzheimer’s disease,” said Cairns.
This indicates a potential new direction in post-concussion care, aimed at preventing long-term damage often linked to repeated head trauma.
A revolutionary brain model
David Kaplan, Stern Professor of Engineering at Tufts and co-author of the study, emphasized the importance of their laboratory brain model.
“The brain tissue model takes us to another level in studying the links between injury, infection and Alzheimer’s disease,” he said.
This model allows researchers to recreate a realistic brain environment in which they can monitor virus behavior, plaque formation, and inflammatory responses in response to simulated trauma.
“There is extensive epidemiological evidence on environmental and other links to Alzheimer’s disease risk. The tissue model will help us put this information on a mechanistic basis and provide a starting point for testing new drugs,” he added.
The model thus constitutes a crucial tool to bridge the gap between large-scale health data and the specific biological processes behind neurodegenerative diseases.
Targeted interventions for concussions
The study results highlight the potential of antiviral or anti-inflammatory treatments following head trauma to prevent the reactivation of latent viruses such as HSV-1.
This approach could reduce the risk of developing neurodegenerative diseases later in life. Additionally, the research highlights the broader importance of understanding how environmental factors and bodily responses interact after trauma.
As scientists continue to refine these brain models and study in more detail how concussions affect brain chemistry, they hope to develop targeted interventions.
Such advances could not only benefit athletes, but also countless people around the world who suffer from traumatic brain injuries, potentially transforming post-injury care and long-term health outcomes.
—–
Do you like what you read? Subscribe to our newsletter for engaging articles, exclusive content and the latest updates.
Check us out on EarthSnap, a free app brought to you by Eric Ralls and Earth.com.
—–