Boston – Regarding weight measurement, BMI is the acronym that everyone likes to hate. Health professionals have long used body mass index as a quick screening tool to speed up certain patients in a “red code” management plan – people whose weight endorses them with future health problems.
The problem is that the BRI measures the risk for health by calculating size and weight. However, muscles and bones weigh more than fats, so that BMI measures can overestimate the danger for people with muscle construction or a larger frame. Conversely, the BMI can underestimate health problems in the elderly and anyone who has lost muscles, according to the Harvard Th Chan School of Public Health in Boston.
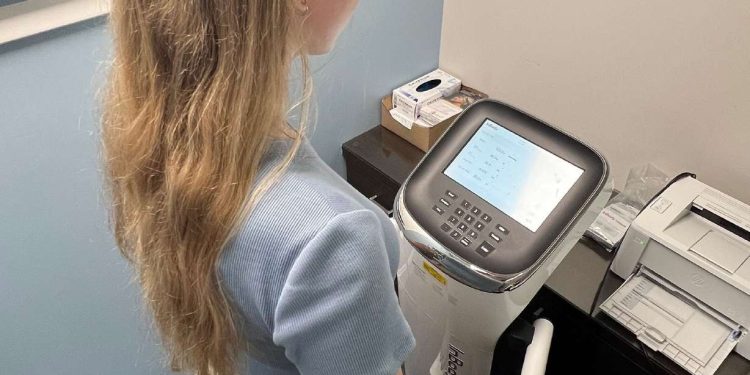
Now, the authors of a new study say that a different approach to weight measurement could be a more precise way to predict future health problems. Analysis of the bioelectric impedance, or BIA, uses undetectable electric currents to measure not only the percentage of body fat but also the muscle mass and the weight of the water.
The technology works like this: you stand on metal plates on the machine while holding your hands or thumbs on another metallic attachment from the body. Once started, the machine sends a low electric current through the body. Body fat, muscles and bones all have a different electrical conductivity, so that the machine uses algorithms to determine lean muscle mass, percentage of body fat and water weight.
“We found that the percentage of body fat was a stronger predictor of the risk of mortality at 15 years in adults aged 20 to 49 that BMI,” said Arch Mainous III, the main study of the study published Tuesday in the journal Annals of Family Medicine.
Regarding the death of heart disease, people with high body fat as measured by BIA were 262% more likely to die than people who had a healthy percentage of body fat, said Mainous, professor and vice-president of community research and family medicine at the University of Florida Medical School.
“Now, remember, the use of BMI has not reported risk at all in this younger population, which is not that which we generally consider at high risk of heart disease,” said Dr. Frank Orlando, principal author, associate professor of community health and family medicine at the University of Florida.
“Think of the interventions we can do to keep them healthy when we know it early. I think that changes the situation of how we have to look at the body composition,” said Orlando.
The problem with BMI
The BMI is measured by dividing your weight by the square of your size. (If you are mathematically challenged like me, the National Institutes of Health have a free calculator.)
In the world of the BMI, a body mass between 18.5 and 24.9 is a healthy weight, between 25 and 29.9 is overweight, between 30 and 34.9 is obese, between 35 and 39.9 is class 2 obesity, and all that is greater than 40 is “severe” or class 3 obesity. People are considered as a weight insufficiency if their BMI is less than 18.5.
The use of BMI to measure health risk work – at the level of the population. Innumerable studies have shown that a higher BMI is really correlated with the development of chronic diseases of all kinds – cancer, heart disease, type 2 diabetes, kidney and hepatic diseases, etc.
Where the BMI fails is at the patient’s level. Imagine a patient who is “thin” – thin outside but riddled with fat globes rolled up around major organs inside. Your BMI would be good even if your health was in danger.
“These people are more likely to have a non -alcoholic liver disease, more likely to have a high glucose, more likely to have high blood pressure and more likely to have inflammation in general,” said Mainous.
All these health problems can be treated, arrested and, in some cases, even inverted if they are taken early, he added.
I think that changes the situation of how we have to look at the body composition.
–Dr. Frank Orlando, Associate Professor of Clinic at the University of Florida Health
Although doctors are aware of the problems with the BMI, many prefer it “because it is cheap and easily put into practice,” said Mainous. “They would like to use a more direct measurement like a Dexa scan, but they cost too much and are not widely available, so everyone falls to the indirect measure of the BMI.”
Dexa means the double energy x-ray absorptiometry and is the ordeal for body mass analysis. These machines can cost between $ 45,000 and $ 80,000, so patients are generally going to the hospital or a specialized center to get the scan, said Orlando. The cost for the patient can easily be $ 400 to $ 500 per scan, he said.
“However, we have found that the more recent versions of the bioelectric impedance are quite precise, giving valid and reliable results,” said Orlando.
A note – Bioelectric impedance products are not as precise, said Dr. Andrew Freeman, director of prevention and cardiovascular well -being at National Jewish Health in Denver.
“They can be very affected by the amount of body fluid you have, how hydrated you are,” said Freeman, who was not involved in the new research. “Home measures will only give a stage – the machines based on the clinic are more precise.”
Is it time for doctors to adopt body fat measures?
The new study analyzed data on 4,252 men and women who participated in the federal survey from 1999 to 2004 called Nhanes, or in the National Health and Nutrition Examination Survey, an annual health examination of the country.
The technicians measured the body composition of each person, including the size, the weight and the waist. In addition, all participants have undergone an analysis of bioelectric impedance based on a clinic, which measures the resistance of the body to electric currents.
The researchers then compared this data with the national index of deaths until 2019 to see how many people died. After adjusting age, breed and poverty status, the study revealed that a BMI which qualified someone obesin was associated with a risk of statistically significant death of the cause, compared to those of the healthy distribution area of the BMI.
People with high body fat as measured by bioimpédance analysis, however, was 78% more likely to die of any cause, said Mainous. The measurement of the waist tower was also useful, but not as precise as body mass.
Add this to the chances of 262% higher to die of a heart disease found by the study, and it is obvious for doctors to use a bioelectric impedance analysis, said Orlando.
The main dishes to remember from this article were generated with the help of large languages models and examined by our editorial team. The article, itself, is only written by man.