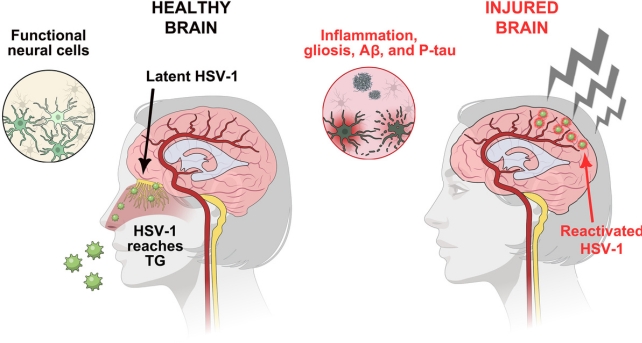
A severe blow to the head can also deal an insidious blow to the human immune system – a double blow that could awaken dormant viruses in the body, potentially contributing to neurodegenerative disease.
A study using stem cell ‘mini-brains’ has shown that a herpes simplex virus 1 (HSV-1) infection already ‘stopped’ by the immune system can break free of its chains when brain tissue is injured.
“We thought: What would happen if we subjected the brain tissue model to a physical disturbance, something akin to a concussion?” says biomedical engineer Dana Cairns of Tufts University in the United States.
“Would HSV-1 wake up and trigger the neurodegeneration process?
The answer seems to be yes. Although these mini-brains are not perfect representations of a real brain, they are good models of how brain tissue may respond when subjected to repeated light blows to a “closed head.”
A week after the injury, the researchers noticed the formation of protein clumps and tangles in the brain tissue, characteristic of neurodegenerative diseases such as Alzheimer’s.
Some brain cells also showed damage related to neuroinflammation, and there was a significant increase in the number of pro-inflammatory immune cells.
Head injuries, including chronic traumatic encephalopathy (CTE), have recently emerged as a major risk factor for neurodegenerative diseases, and preliminary research suggests that chronic inflammation caused by even mild head trauma may play a role. role in cumulative damage.
It’s not yet clear how this process takes place, but other recent studies have shown that viruses may play a unique role. HSV-1 is a major risk factor for neurodegeneration, potentially doubling the risk of developing dementia.
In a 2008 study, researchers found that HSV-1 genes were present in 90% of protein plaques in the postmortem brains of Alzheimer’s patients. The majority of this viral DNA was found in the plaques.
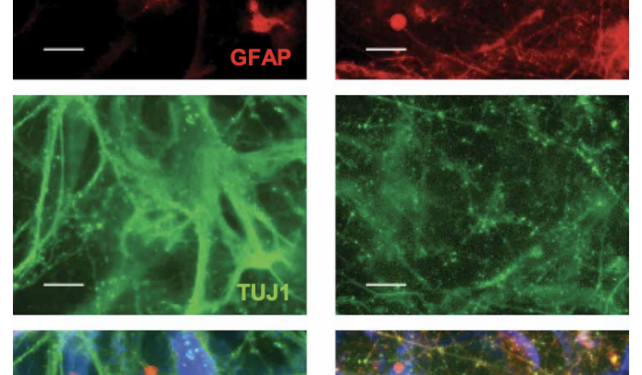
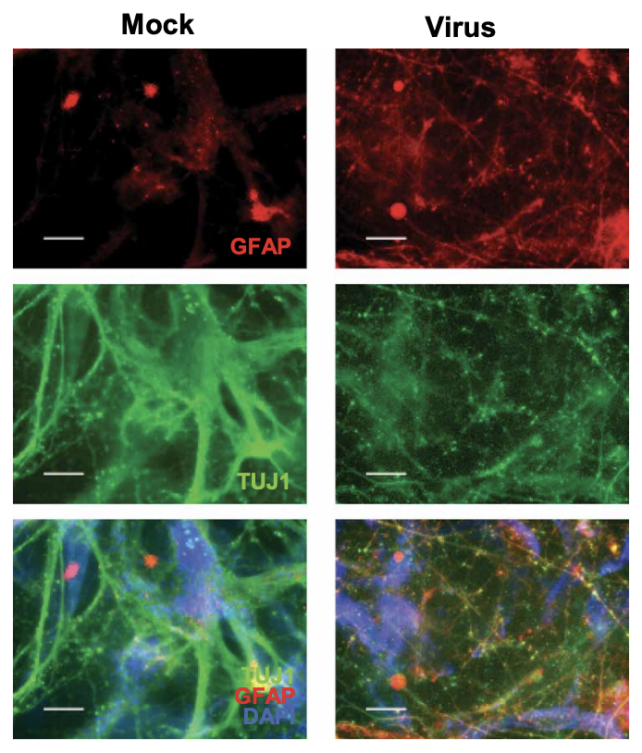
To further study whether brain injury could reactivate HSV-1 infection, researchers at Tufts University and the University of Oxford turned to isolated brain slices. In response to physical injury, people infected with latent HSV-1 secreted significantly less of the excitatory neurotransmitter, glutamate.
The 8-week-old mini-brains fared better after injury than the 4-week-old ones, indicating that head trauma may have more profound effects on young, developing brains.
“Our results show that TBI causes reactivation of latent HSV-1 in our 3D brain model… and that if the injury is repeated, the damage is much greater than after a single hit,” the team concludes.
Whether HSV-1 is awakened by physical damage or by another pathogen, Cairns and his colleagues suspect that this extremely common virus is a contributing factor in the development of dementia.
They argue that future studies should “investigate possible ways to mitigate or stop the damage caused by head trauma, such as anti-inflammatory and antiviral treatment after injury, thereby preventing reactivation of HSV-1 in the brain and reducing the further development of Alzheimer’s disease. »
The study was published in Scientific signage.