How this COVID-19 surge became the worst in years in California. ‘It came out of nowhere’
California’s strongest summer COVID surge in years continues to rage, and an unusual midsummer mutation may be partly to blame.
Experts say several factors may be behind the biggest surge in summer infections since 2022. A series of heat waves and smoke from devastating wildfires have forced many Californians to stay home, where the disease can spread more easily. Most adults are also far from their last contact with the coronavirus, or their last dose of the vaccine, meaning they are more vulnerable to infection.
But changes in the virus have also widened the scale of the wave.
Of particular concern is the emergence of a hyperinfectious subvariant known as KP.3.1.1, which is so contagious that even people who have escaped infection throughout the pandemic are falling ill.
“COVID is extremely common today,” said Dr. Elizabeth Hudson, regional infectious disease chief for Kaiser Permanente’s 16-hospital Southern California health system.
COVID-19 hospitalizations are rising but remain below the peaks of the last two summers, likely thanks to some residual immunity and the widespread availability of anti-COVID drugs such as Paxlovid.
The World Health Organization has warned of rising COVID-19 infections worldwide and expressed concern about the emergence of more severe variants.
“In recent months, regardless of the season, many countries have experienced outbreaks of COVID-19, including during the Olympic Games,” said Dr Maria Van Kerkhove, WHO technical lead for COVID.
Among those taken into care was 27-year-old American sprinter Noah Lyles, who after winning gold in the men’s 100-meter final failed Thursday in the 200-meter final, taking bronze. Lyles collapsed after the race, suffering from shortness of breath and chest pains, and was later taken away in a wheelchair.
“It definitely affected my performance,” he said of the illness, estimating he felt “90 or 95 percent” of his full strength.
The coronavirus test positivity rate has been rising for weeks, topping 10% globally and 20% in Europe. In California, the coronavirus test positivity rate was 14.3% for the week ending August 5, surpassing peaks from last summer and winter and up from 10% last month.
There were already indications in May that the typical mid-year surge in the United States was starting early, as a pair of new coronavirus subvariants — KP.2 and KP.1.1, collectively dubbed FLiRT — began to make a splash, replacing the dominant winter strain, JN.1.
But by July, a descendant strain, KP.3.1.1, had clearly taken flight.
“KP.3.1.1 is extremely transmissible and a little more immune-evasive. It emerged unexpectedly in the summer,” said Dr. Peter Chin-Hong, an infectious disease specialist at the University of California, San Francisco.
Cases are up at Kaiser Permanente Southern California, and “looking at the CDC data … KP.3.1.1 is really what’s driving this particular increase,” Hudson said. “We’re definitely up significantly from last summer.”
Anecdotally, some people who are infected report being “pretty miserable, actually – really intense fatigue for the first couple of days,” Hudson said.
People might think their symptoms are just allergies, she said, but “it’s probably COVID. So we really encourage people to continue to get tested.”
An initial negative test doesn’t necessarily mean you’re in the clear. Officials recommend repeat testing up to five days after symptoms appear to be safe.
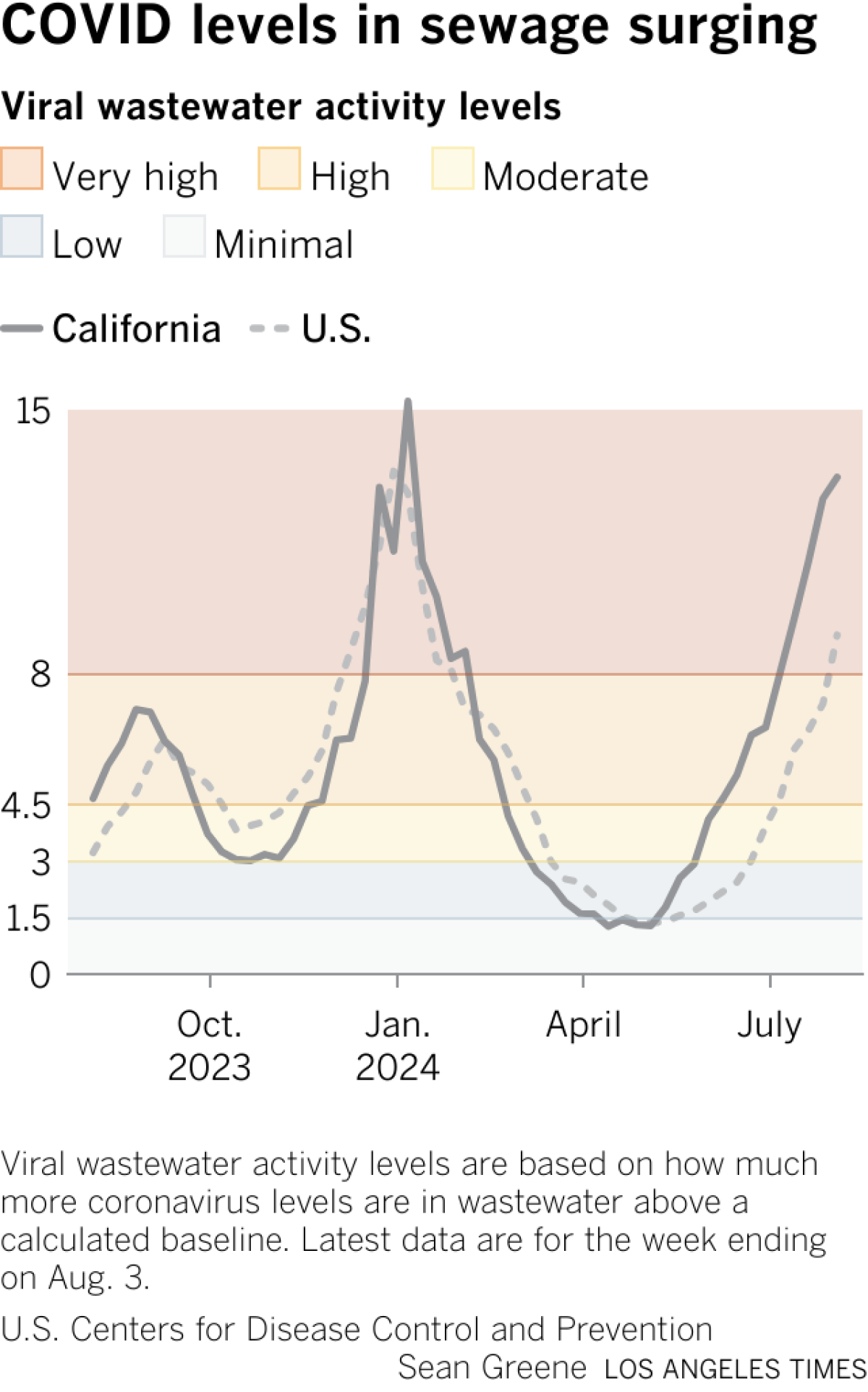
California has now reported four consecutive weeks of “very high” levels of coronavirus in its wastewater, according to data released Friday by the U.S. Centers for Disease Control and Prevention (CDC). That follows five weeks of “high” virus levels.
Last summer, California had only eight weeks with “high” levels of coronavirus in wastewater, and never reached “very high” levels. In the summer of 2022, California had 16 weeks with “high” or “very high” levels of coronavirus in wastewater.
“Fewer people have been vaccinated this year than last year at this time,” Chin-Hong said. “That means older people, in particular, are just not equipped to deal with this virus.”
According to the CDC, 44 states have “high” or “very high” levels of coronavirus in their wastewater. Five states and the District of Columbia have “moderate” levels, and there is no data for North Dakota.
The CDC said coronavirus infections are “increasing” or “likely increasing” in 32 states, including California; are “stable or uncertain” in seven states, as well as the District of Columbia; are “likely decreasing” in Connecticut; and are “declining” in Hawaii and Nevada. No estimates have been made in eight states.
In Los Angeles County, coronavirus levels in wastewater climbed to 54% of last winter’s peak during the 10-day period ending July 27, the most recent available. A week earlier, coronavirus levels in wastewater were at 44% of last winter’s peak.
For the week ending Aug. 4, Los Angeles County reported an average of 479 coronavirus cases per day, double the number recorded five weeks earlier. The cases are an undercount because they reflect only tests conducted at medical facilities, not self-tests conducted at home.
In Santa Clara County, the most populous county in the San Francisco Bay Area, coronavirus levels were high in all sewers, including those in San Jose and Palo Alto.
Coronavirus-related hospitalizations and emergency room visits are also up. In the week ending Aug. 3, there were an average of 403 people with coronavirus in Los Angeles County hospitals per day. That’s double the number from five weeks earlier, but still about 70% of last summer’s peak and a third of the peak seen in the summer of 2022.
In the week ending Aug. 4, 4% of emergency room visits in Los Angeles County were classified as coronavirus-related, more than double the number recorded seven weeks earlier. The peak last summer was 5.1%.
“We’ve had a few people who have gotten very sick with COVID. These are people who tend to be pretty severely immunocompromised,” Hudson said.
The University of California, San Francisco, has also seen an increase in the number of hospitalized patients infected with the coronavirus. As of Friday, there were 28, up from fewer than 20 a week earlier, Chin-Hong said.
In the San Francisco Bay Area, three counties have urged more people to consider wearing masks in indoor public settings because of the COVID surge. The Contra Costa County Department of Public Health “recommends wearing masks in crowded indoor settings, especially for people at high risk of severe illness if infected,” the agency said Tuesday, following similar calls from health officials in San Francisco and Marin County.
Compared to advice such as washing hands and staying away from sick people, suggesting wearing a mask may provoke strong opposition from some.
“As soon as people see that, in their minds it sets off a chain reaction of all the negative aspects of the pandemic, like the shutdown of society and social isolation,” said Dr. Abraar Karan, a physician and infectious disease researcher at Stanford University.
But masks help reduce the risk of infection, and people don’t need to wear them all the time to benefit. Karan says he socializes with people and eats at restaurants indoors. But he chooses to wear a mask in other situations, like “when I travel” and, of course, at work.
Doctors say wearing a mask is one of many tools people can use to reduce their risk, and may be especially helpful in crowded indoor settings.
Karan said he has seen more coronavirus-positive patients while working shifts in the emergency room, and he suggested that more health care providers take the time to order tests. He said he worries that when people come in with relatively mild symptoms, they will be sent home without being tested.
But that could miss a potential COVID diagnosis, which could allow a patient to get a prescription for an antiviral drug like Paxlovid.
Without testing, “you run the risk of cutting corners and not prescribing people medications that they technically should be getting,” Karan said.
Times reporter David Wharton contributed to this report from Saint-Denis, France.




