Karla Flores was 18 years old when she started to live a double vision. She knew something was wrong but had trouble finding a diagnosis. Finally, she saw an ophthalmologist who referred it to a neurosurgeon.
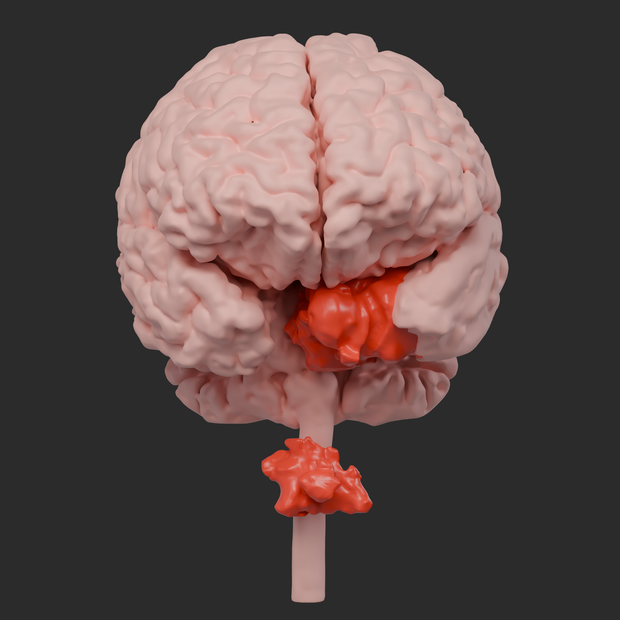
Flores, then 19 years old, was diagnosed with a chordomed rolled around his brainstem. Chordomas are incredibly rare – only about 300 are diagnosed per year in the United States, according to Cleveland Clinic – And they are slow growth tumors.
The tumor exerted pressure on several of the heads of Flores, said Dr. Mohamed Labib, a neurosurgeon from the University of Maryland University who led his treatment. Labib has developed a complex surgical plan which required two surgeries to eliminate the tumor without damaging the delicate nerves.
When Flores suffered an MRI in the morning of the first surgical intervention, the technician positioned the camera a little lower than necessary. Looking at the scans, Labib realized that Flores had a second chordoma. He was at the top of his spine, at the front of his spinal cord. He was wrapped around his spinal cord and had invaded the vertebrae in his neck, said Labib.
“They told me that if they hadn’t seen it, I could have been paralyzed,” Flores told CBS News.
Medical Center of the University of Maryland
Despite the surprising discovery, Labib decided to move forward with the procedures to eliminate the first Chordoma of Flores. The tumor was successfully removed by a traditional neurosurgery and another procedure that crossed the Nose of Flores.
Between the procedures, Labib studied the location of the second tumor. In most cases, he would make an incision in the spine to approach the tumor from the rear, but the location of the chordoma meant that it was not an option. Going through Flores’s nose again would no longer give it space to work. A colleague even suggested that there was nothing that they could do.
“I spoke to colleagues, and one of them said” you will not heal it “, basically, maybe she should be more a patient in palliative care,” said Labib.
Palliative care refers to the creation of a comfortable terminal patient for their last days. “I was not very enthusiastic about this,” added Labib.
Develop a unique surgical plan
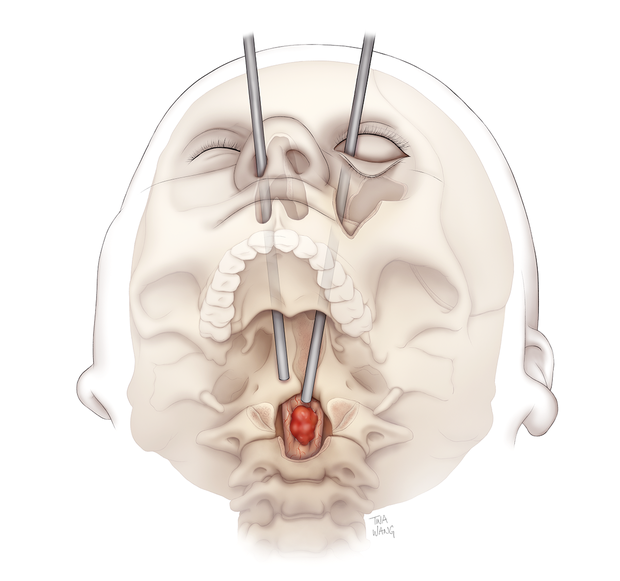
Labib continued to study the Flores scans and seek ways to reach the second chordoma. While considering approaching him by the nose, he realized that the cheekbone between his nose and the eye was one of the obstacles that prevented him from reaching the tumor. That gave him an idea: what if he approached Flores’s eye?
He had done it for surgery several years ago, but never to eliminate a vertebral tumor. Labib spent weeks practicing technique, which he called the “third nostril” approach in the UMMC neurosurgery laboratory. He used corpse heads and skull models to ensure that he could reach and safely operate the tumor. He and other members of the Flores team spent weeks solving potential problems, including ensuring that they could create surgical opening without damaging his eye globe and modify the surgical instruments so that they work for the procedure.
Medical Center of the University of Maryland
After being confident in the approach, Labib spoke to Flores and his family family.
“His mother cried. Karla was emotional. His father, he is not an emotional guy, but you could see his silence that he was worried,” recalls Labib.
Flores said she had trusted Labib and approved surgery.
“I was afraid of not seeing my parents again, because you never know what will happen when you enter surgery,” she admitted.
In the operating room, the plastic and reconstructive surgeon for the face, Dr. Kalpesth T. Vakharia, cut through the membrane which protects the eye inside the lower eyelid and removed the bottom of the flora eyes and part of his cheekbone. This allowed Labib to reach the operating site. He also left Flores without external scars, said Vakharia.
Once the bones have been removed, the head and neck surgeon of the head and neck, Dr. Andrea Hebert, pierced by the vertebrae of Flores to reach the tumor. They dissected it carefully, following the procedure they had developed in the laboratory. As they were finished, the chordoma was completely deleted, said Labib.
“It was perfect,” he said.
Once done, Vakharia has rebuilt the socket of flora’s eyes with a titanium plate and rebuilt its cheek with its hip bone. The process has taken about 20 hours, said Labib.
“Each step is an accomplishment”
The chordoma was removed, but Flores had even more treatment to come. A spine surgeon stabilized the vertebrae who had been affected during surgery. Six weeks later, she suffered radiotherapy to make sure that there was no cancer in her body. Almost a year after completing the treatment, Flores has no evidence of cancer.
The treatment was followed by rehabilitation therapy. Flores, now 20 years old, has trouble moving his left eye due to the chordoma nerve lesions, but continues to work on physiotherapy.
Karla Flores
Flores said that when she felt better, she wanted to go to school to become a manicure. She has follow-up meetings at the UMMC every few months. Her biggest fight at the moment is medical bills: she said she owed about $ 600,000. A gofundme only collected a few thousand dollars.
“I don’t stop remembering to take one day both and know that each step is an accomplishment. I am also happy to have held the field and that I continued to look for help until I find it,” said Flores in a statement sent by email.
Labib said that he hoped that the procedure can be used to help operate other tumors that are difficult to reach.
“I think this opens a new corridor for the approach of the tumors in the upper cervical (or the high part of the) Vertebral column,” said Labib. “I think this third approach to nostrils is a smaller, easier and cleaner approach, and I think it will really adopt these difficult tumors in front of the spinal cord.”